instantvob®
- Modernized Benefit Verification for Providers
Providers Like You are Saving Hours Every Single Day!
If You’re Tired of Being Stuck on Hold, You’ve Come to the Right Place!
When we say instant, we mean instant—immediate access to patient insurance benefit benefit information when you need it.
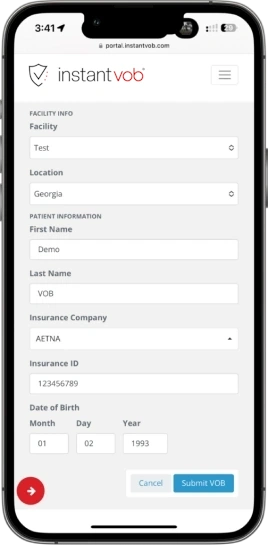
Elevate your decision-making process for patient admissions and treatments with instantvob®. Our solution, designed with a mobile-first approach, revolutionizes the way healthcare and revenue cycle management teams operate, saving countless hours.
Looking to Integrate instantvob® into Your WordPress Site or Your Own Software?
Access Benefits Data Anytime, Anywhere
Round-the-Clock Availability
Intuitive Multi-Device Access
Access patient coverage details instantly on any device, whether desktop, tablet or mobile, for confident decision-making anytime. Our mobile-first design ensures an intuitive experience across platforms. The streamlined interface allows effortless navigation and fast verification, whether at your desk or on the go.
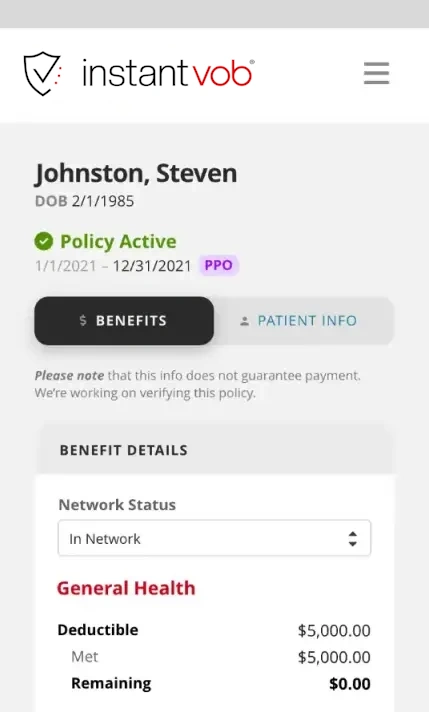
Policy Status
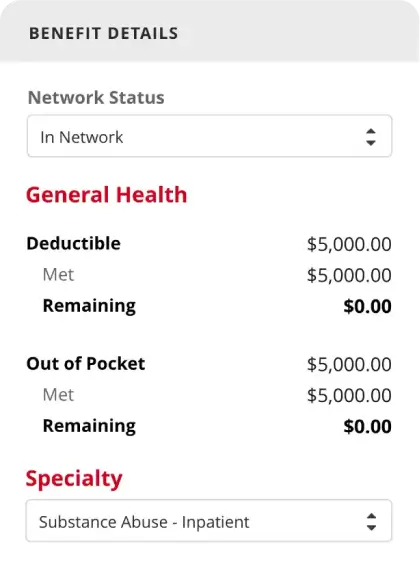
In-/Out-of-Network Deductibles
One Unified Platform
Seamless User Experience
Technology should streamline — not complicate — healthcare administration.
Our platform stands out for its accuracy, simplicity, and compliance. It’s designed to be always available, catering to the 24/7 nature of healthcare decision-making and patient care.
Accelerate Admissions with Crucial Insights
Built for the Unique Needs of Healthcare
Allergy Testing and Treatment
Anesthesia Services
ASC Facility
Chiropractic Care
Diagnostic Services
Emergency Services
Fertility Services
General Practitioners
Home Health Care
Hospice Care
Immunization Treatment
Maternity Care
Mental Health Services
Occupational Therapy
Optometry (Vision)
Pharmacy Services
Physical Therapy
Podiatry
Psychotherapy
Radiation Therapy
Routine Physicals
Skilled Nursing Facility
Specialist Services
Substance Abuse Treatment
Telemedicine Services
Urgent Care
X-Ray Services
instantvob® Offers Your Organization The Benefits Of A Cloud-Based Digital Revolution:
- Intuitive User Experience: With a mobile-first interface designed for effortless navigation and fast verification across devices
- Instantaneous Verification of Benefits: Allowing providers to make timely admissions decisions
- Round-the-Clock Access: To active status, deductibles, coverage alerts, and more
- Healthcare-Specific Design: For hospitals, substance use facilities, mental health facilities, individual practitioners, and more
- Fast, Simple, Accurate, & HIPAA Compliant: Requiring only five patient identifiers for comprehensive results
- Streamlined Processes: To simplify operations, reduce collection issues, and enhance patient outcomes
Imagine healthcare software that simply clicks.
That’s the future we’re building at instantvob®. A future where tangled processes unravel, freeing healthcare providers to focus on what they do best: patient care.
Key Features of instantvob® :
- Access to multiple data sources for unparalleled accuracy
- An intuitive interface with productivity-enhancing tools
- Customizable reporting for compliance
- Comprehensive data and access security
- Mobile optimization for on-the-go access
- Continuous security and performance enhancements
- Dedicated US-based support via email and phone
- Powered by Amazon Web Services
Simplify initial patient encounters with instantvob®, taking charge of the process for a quicker, more accurate, and efficient workflow.
Effortless Integration for Streamlined Workflows
Cloud-Based, Comprehensive Data Solution
With just five patient identifiers, instantvob® responds in real time with extensive VOB data, including:
- Patient deductible details
- Out-of-pocket costs
- Coverage across various healthcare specialties
- Policy active status
- Patient demographic information
Experience the benefits of our cloud-based tool designed to streamline the verification process for healthcare providers across various sectors, enabling swift, informed decisions on patient admissions and treatments.
Because exceptional healthcare deserves exceptional tools.
What Healthcare Professionals Say About Us
“Verification of benefits on nights and weekends has increased my intakes dramatically.”
– Tony G.
“Benefit verification at this cost is a game changer.”
– Charles G.
“I was making some wrong decisions with admissions, instantvob® has helped me make the right calls.”
– Caulder H.
“We began using instantvob® as an overflow option for our admissions team after hours and on weekends. We find this tool helpful and very easy to use. instantvob® assists us in making important financial decisions by providing benefits information immediately. It’s important to us that our clients are not left waiting for admission until we can complete a live verification”.
– Maura O.
Discover More
Frequently Asked Questions
Our standard service plan is $149.99/month. Pricing is scheduled on a per-unit basis for volume that exceeds the standard service plan total.
Visit https://portal.instantvob.com/sign-up to sign up today!
Login at https://portal.instantvob.com/ and begin submitting your verification of benefits request.
Pricing information is available at https://instantvob.com/pricing.
We offer a monthly recurring subscription at $149.99/mo.

